
LexisNexis® Intelligent Investigator™ is designed to provide a lens into the unknown in post-paid claims by making connections others can’t make. Built exclusively for healthcare investigative teams, it uses sophisticated rules-based analytics to detect fraud, waste, and abuse and prioritize the cases that are potentially most lucrative.
Featured Assets
Client Case Study: Download the Case Study to learn how one health plan’s fraud investigators used LexisNexis® Intelligent Investigator™ to analyze medical and pharmacy claims — and turn mountains of data into the precise intelligence they needed. LexisNexis® Intelligent Investigator™ showed them the extent of the problem — so they could act immediately to fix it — by pinpointing suspicious behavior across all claim types.
Executive Summary: Enrollment fraud is a serious and growing problem. Health plan leaders know how easy it is for identities to be compromised. They must setup their efforts to guard against the financial losses, negative press, compliance problems and other challenges that can result from fraudulent enrollment. Download the Executive Summary to learn about our systematic approach for combating fraud.
Want to stop the flow of healthcare fraud? Call now to speak with one of our solutions experts at 866.396.7703.

Download Featured Assets
Please select asset below to download.-

CASE STUDY: Intelligence you can access when you need it is intelligence you can use.
-
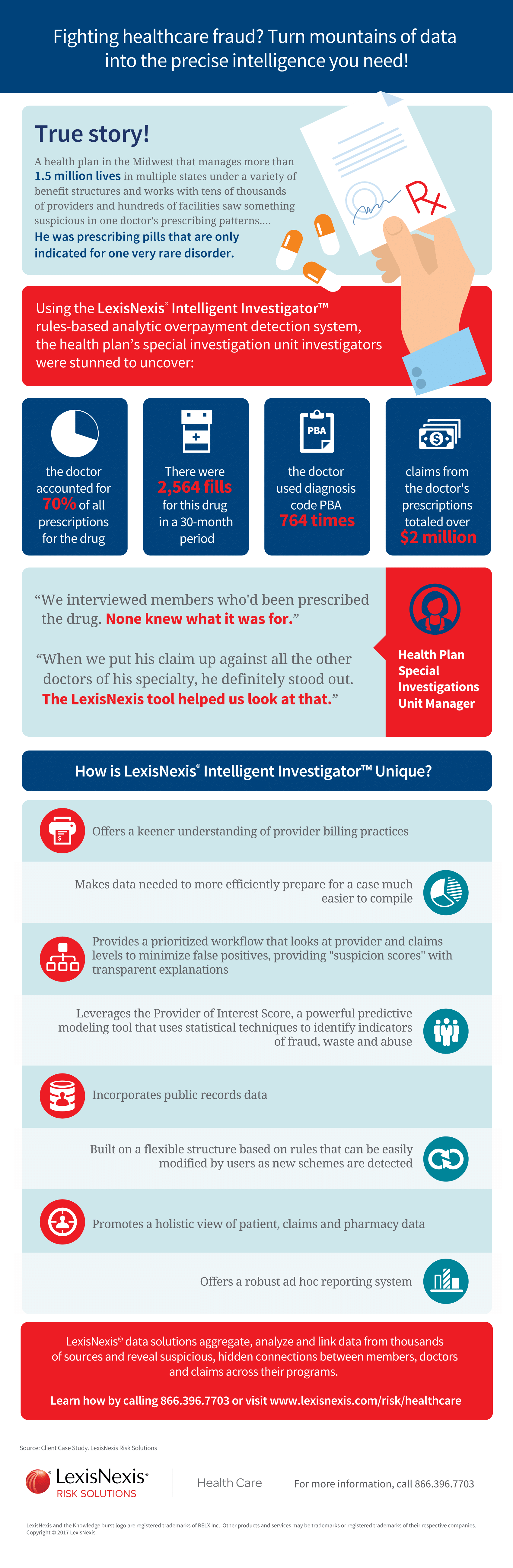
INFOGRAPHIC: Fighting healthcare fraud? Turn mountains of data into the precise intelligence you need!
-
Executive Summary: Considering a new tactic? Learn about a systematic approach for combating enrollment fraud.

